Findings in the physical neurological examination as an indicator of Alzheimer's disease progression
Patients with cognitive disorders such as memory loss often also show conspicuities in the clinical neurological examination. This correlation can be used to predict the development of the disease, as researchers from the DZNE in Munich have now shown.
The findings of neurological examinations could have a more far-reaching influence on the treatment of patients with Alzheimer's disease: Conspicuities in physical neurological examinations, such as gait disturbance or increased deep tendon reflexes, are apparently closely related to the progression of the disease. "Approximately two-thirds of the Alzheimer's patients studied showed abnormalities in the non-cognitive neurological examination," says Dr. Jonathan Vöglein, who conducts research at the German Center for Neurodegenerative Diseases (DZNE) in Munich and is first author of the study, which now appears in the renowned journal Alzheimer's & Dementia.
For their work, the scientists led by Jonathan Vöglein and Johannes Levin, professor of clinical neurodegeneration at the DZNE in Munich and LMU Klinikum, used data from the worldwide observational study DIAN ("Dominantly Inherited Alzheimer Network"). This study examines people who have a rare hereditary variant of Alzheimer's disease or who have a greatly increased risk for the disease. "Symptom onset of autosomal dominant Alzheimer's disease is on average in the early to mid-40s. This allows for an investigation of Alzheimer’s disease independent from age-associated comorbidities" explains Jonathan Vöglein, who also works as a neurologist at the LMU Klinikum in Munich. In the sporadic form of Alzheimer's, patients are often already older than 70 when they become ill - and in many cases have physical limitations due to their age. This makes it difficult to assess whether abnormalities in the neurological examination are caused by Alzheimer's disease - or whether they are due to concomitant diseases. In contrast, the much younger patients who now formed the basis for the new examination are mostly physically fit when they develop dementia. This means that conspicuous neurological examination findings can be more clearly attributed to Alzheimer's disease.
The neurological examination is part of the standard repertoire for neurologists. It includes amongst others the examination of cranial nerves, motor strength, deep tendon reflexes, coordination and sensory testing. "The clinical neurological examination, along with taking a medical history, forms the basis for treating people with nervous system disorders," Levin explains. Until now, however, it has not been evaluated whether findings in this classic examination could be related to Alzheimer's disease. Vöglein and Levin, together with their colleagues, now found that two-thirds of the young participants in the DIAN study had abnormal neurological findings. Common findings include increased deep tendon reflexes, gait disturbance, tremor, increased muscle tone, and saccadic smooth pursuit eye movement.
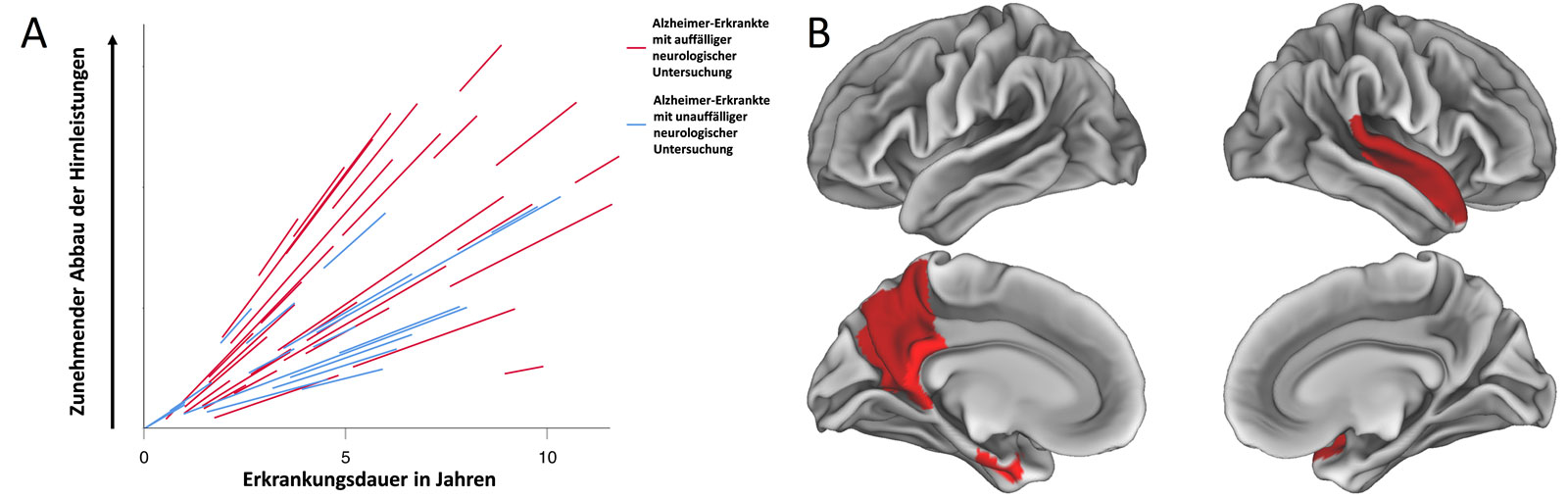
The authors of the study found that if there are abnormal findings in the physical neurological examination, the cognitive impairment is more pronounced. "It turned out that abnormalities in the neurological examination are accompanied by poorer cognitive performance and can even be helpful in predicting a more severe course of the disease," says Johannes Levin. Put simply, if findings in the physical neurological examination are present, Alzheimer's disease progresses more rapidly. And the differences in progression are remarkable: in the study, cognitive performance deteriorated more than twice as fast in patients with abnormalities in the neurological examination than in those without abnormal examination findings.
The crucial thing about the study is that the results could also be applied to those patients who suffer from the sporadic form of Alzheimer's - and that is the vast majority of cases. "Autosomal dominant and sporadic Alzheimer's disease are very similar. Therefore, if patient age and comorbidities are taken into account,translatability of the results may be possible . In this regard, further investigations are warranted" says Vöglein.
The study by the DZNE researchers may directly benefit Alzheimer's patients in the future: So far, there are hardly any indicators that can be used to predict the course of the disease. However, the more precisely this can be done, the better doctors will be able to tailor the treatment plan.
Original publication
Pattern and implications of neurological examination findings in autosomal dominant Alzheimer disease.
Jonathan Vöglein et. al.
Alzheimer’s & Dementia (2022).
DOI: 10.1002/alz.12684
