Dementia
The silent pandemic
Some of the negative effects of demographic change in our society have been revealed by the Corona pandemic – and in a particularly painfully way. The spread of the Sars-Cov-2 virus has taken a heavy toll on human lives, especially among the elderly population. Once again, and in all clarity this underlines what we have all known for a long time anyway: that a population’s aging goes hand in hand with a higher diseasy susceptibility. However, it also became clear that overcrowding hospitals with seriously ill patients can lead to considerable delays in the care of other patients.
In the long term, it is precisely these people with serious illnesses who will place a burden on the healthcare system, both socially and economically. To date, more than 2.5 million people in Germany have tested positive for Covid-19; of these, tragically, more than 72,000 have died. At the moment, it is difficult to estimate how many more suffering from acute or chronic illnesses have not received appropriate treatment due to the Corona emergency. Also difficult to estimate is the number of treatments that were actually planned but then postponed in order to prevent or avoid acute illnesses such as heart attacks.
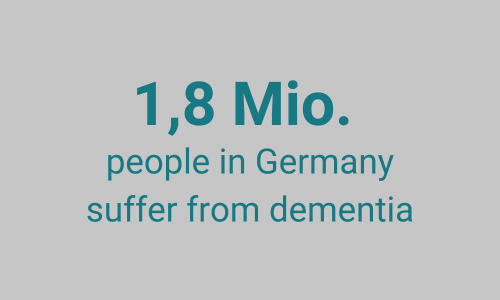
As of today, 1.8 million Germans, mostly elderly, are affected by dementia and about 250,000 by Parkinson's disease. Unfortunately, since effective therapies to slow or reverse the progression of either disease are still not really available, the majority of these patients will die from it. Also carework for them interferes with the lives and activities of numerous others every day. The number of families and professional caregivers involved in the care of people with neurodegenerative diseases can easily be three times as hight as the number of people affected by dementia and other neurodegenerative diseases.

In Germany, the total annual cost for the medical and carework fora person with dementia amounts to approximately €44,600. 46% of these are direct medical costs, covered by health or long-term care insurance, and 54% are indirect costs such as the equivalent of time spent by family caregivers and their "productivity losses" due to reduced working hours in employment. Overall, healthcare expenditures for people with dementia in Germany have increased disproportionately in recent years and currently account for 36% of total social costs for the over-65s. Compared to other diseases, these costs are very likely to continue to rise disproportionately in the coming years. By 2060, the costs of dementia could amount to €195 billion euros per year, accounting for 48% of the total social costs for the over-65s.
Add to this the fact that virtually all dementia patients develop comorbidities requiring professional care and hospitalization, and it is not difficult to imagine what lies ahead for the German healthcare system: If the number of dementia patients is expected to reach 3 million in the next few decades, we will face a problem likely to be even more serious than the current covid crisis.
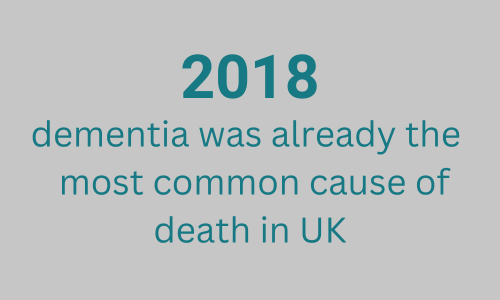
Without effective prevention or treatment, the number of dementia cases will steadily increase. Combined with the non-existence of treatments, this increase in dementia has already led to a dramatic increase in deaths due to dementia. For example, in the UK, dementia was found to be the leading cause of death for the first time in 2018. What is striking is that for other common diseases, where many years of investment in research and drug development have led to successes in both treatment and prevention, the trend is exactly the opposite: today the number of deaths from diseases such as cancer, strokes or HIV have continued to go down.
Of course, the short-term impact of a contagious disease is not comparable to that of chronic, non-communicable diseases such as cancer, diabetes, and even dementia. Chronic, non-communicable diseases simply do not force lockdowns.
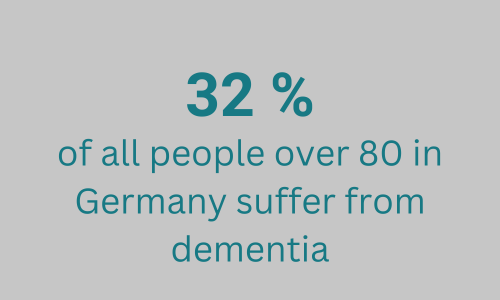
Yet the long-term impact of dementia on society can be immense. Healthcare costs alone already play an enormous role, but so do costs for the German economy and social systems as well - they represent a challenge for society as a whole. Demographic change will lead to a proportional decline of the population of working age, while the proportion of people over 65 will rise significantly. In particular, between the years of 2040 and 2060 the proportion of the very old (older than 80), for whom the probability of developing dementia is at 32%, will increase and, depending on the scenario, in 2060 will account for between 9% and 13% of the total population. The cost of care among the very old is particularly high. Currently, about 70% of people cared for in nursing homes are 80 years and older. The future younger generation will therefore not only have to absorb the declining number of people in work, but will also have to shoulder more care. Overall, it cannot even be ruled out that the costs of the increasing number of dementia cases spread over the years will significantly exceed the costs of the corona epidemic.
The way to solve this “silent epidemic” in the making is to find new strategies for prevention and therapy. Therefore, in 2013 already, the G7 had issued the goal of therapy development by 2025. Unfortunately, we are still a long way from achieving this. The exact causes of neurodegenerative diseases are still unknown to a large degree. Alzheimer's and Parkinson's diseases, as well as other neurodegenerative diseases leading to dementia and motor disorders, start developing decades before symptoms manifest. Therefore, we need tools for early diagnosis and rapid testing of new therapies in specialized clinical research facilities. In addition, we need to implement new strategies in patient care in order to improve the quality of life of those affected and reduce the need for inpatient care.
DZNE’s equipment and impact

DZNE was founded in 2009 by the federal and state governments as the first of the German Centers for Health Research (Deutsche Zentren der Gesundheitsforschung; DZG). The goal was to develop new therapies and prevention strategies as well as new care protocols through highly qualified research. Over the years, DZNE has become a leading institution in research on dementia and other brain diseases. According to an independent evaluation by science publisher Elsevier in 2019, DZNE is one of the world's top ten research institutions in the field of dementia research. In particular, it ranks among the top in the quality of its published papers and in its collaboration with industry partners. Through close collaboration with universities and university hospitals, the first National Clinical Research Platform was created, which can test new drugs in clinical trials. DZNE's Rhineland Study investigates age-related risks for dementia and other diseases among the population. DZNE's Health Care Research Unit has already introduced measures for better management and care of dementia patients into legislation. DZNE has discovered early disease characteristics that allow diagnosis up to 16 years before the disease manifests. New, potentially effective drugs have been and are being developed at DZNE fundamental research. DZNE has established highly characterized patient cohorts at its sites to conduct observational studies and clinical trials based on precision medicine. In addition, DZNE is instrumental in research to develop revolutionary computer architectures such as memory-driven computing as well as AI methods such as swarm learning, which take genomic and other data-intensive research to a new level and make personalized medicine tangible.

Solely based on itsexisting resources, however, DZNE is fighting a losing battle. Major pharmaceutical companies have largely pulled out of developing new Alzheimer's drugs because, in their estimation, it is too expensive. Clinical trials, based on developments over the past 10 years, have continued but have been unsuccessful. Hence, DZNE has developed its own pipeline of potential new drugs awaiting testing in clinical trials. However, specifically the latter are costly and thus cannot be realized with the current resources of the DZNE. It is quite remarkable that the 2013 G7 document on dementia pledged a significant increase in research funding for dementia, but to date the US is the only country to have substantially increased its research budget for dementia. U.S. funding for dementia research has increased sevenfold since 2013 and will reach $3.1 billion in 2021. By comparison, DZNE has a core budget of just under 90 million euros per year - only about 1/10th of the research spending in the U.S. per patient. However, this compares to care costs of 44,600 euros per patient per year in Germany.
