Protein plaques in the brain are the cause of Alzheimer's disease and the starting point for possible therapies. At later stages, however, the disease may become independent from them, report researchers around Prof. Mathias Jucker from Tübingen. Their findings are published in the renowed journal “Nature Communications”.
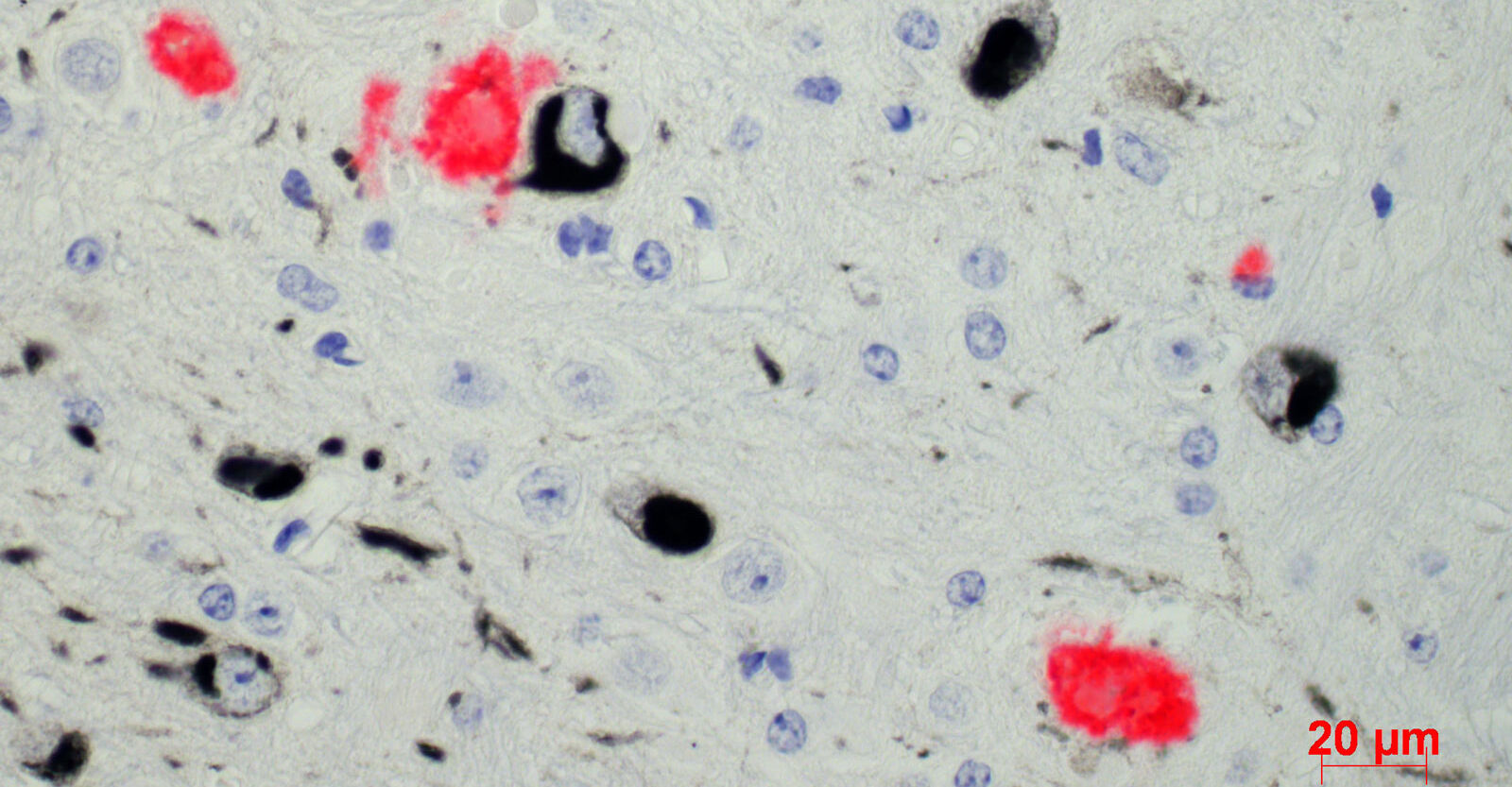
The main cause of Alzheimer's disease appears to be the deposit of a specific protein, beta-amyloid protein, in the brain - according to the current state of Alzheimer's research. The formation of these so-called plaques begins at least twenty years before the first symptoms of the disease appear. So far, however, only a weak correlation has been found between the amount of deposits and clinical symptoms in patients with the disease. The reason for this could be that the disease develops independently of the plaques in progressive stages. This is suggested by a recent study by researchers led by Prof. Mathias Jucker of the DZNE, the Hertie Institute for Clinical Brain Research and the University of Tübingen. Therapy should therefore be started as early as possible, Jucker said. Their findings are published in the renowed journal “Nature Communications”.
"There is convincing evidence that beta-amyloid plaques are the most important cause of Alzheimer's disease," said neurobiologist and principal investigator Jucker. "However, only a weak correlation exists between them and clinical symptoms." For example, he said, the twenty-year delay between the development of the first plaques and the onset of symptoms of the disease is very long. Also, he said, reducing damaging protein deposits in the brains of participants in clinical trials resulted in only a small improvement in their cognitive performance. "All these findings suggested that the Alzheimer's disease cascade could become independent of protein deposits in later stages."
When we reduced the beta-amyloid deposit in early stages, the amount of NfL protein in the cerebrospinal fluid no longer increased.
The Tübingen research team now provides the first experimental evidence that the deposits are uncoupled from downstream neurodegeneration. In their study, they examined mice: In them - as in Alzheimer's patients - beta-amyloid proteins accumulate in the brain with advancing age.
The scientists now specifically reduced the plaques in the mice at different age stages. They then measured another protein in the cerebrospinal fluid of the mice, the so-called neurofilament light chain protein (NfL). The NfL protein is increased in the cerebrospinal fluid of Alzheimer's patients; it is considered an indicator of the degradation of neurons.
The result: "When we reduced the beta-amyloid deposit in early stages, the amount of NfL protein in the cerebrospinal fluid no longer increased. We were able to stop the degradation of the neurons," said Christine Rother, first author of the study. The situation was different at older ages: "When we reduced the formation of beta-amyloid plaques at later stages, the level of NfL protein in the brain water increased without change. Thus, neurons continued to die. Neurodegeneration had decoupled from the deposits," added Ruth Uhlmann, co-first author of the paper.
"So there seem to be two phases of disease progression in Alzheimer's," Jucker concluded. In the first phase, beta-amyloid plaques propelled the disease. At this stage, he said, therapies that counteract the deposits are highly effective. In the second phase, however, neurodegeneration progresses independently of the plaques. Therapies directed against the beta-amyloid plaques now largely miss their mark.
But where is the turning point between the two phases? To get an answer, the research team analyzed the timing of beta-amyloid plaque formation and the rise in NfL protein in the cerebrospinal fluid of presymptomatic participants and mice. The team found that both levels initially rose similarly. "At a certain point, the amount of NfL protein shot up exponentially," Jucker reported. "However, the amount of beta-amyloid plaques did not increase at a similar rate."
This uncoupling of the increase in NfL protein from the formation of beta-amyloid plaques occurred at a time when about half of the subsequent maximum amount of plaques had formed, he said. "That's about 10 years after the first deposits in patients and 10 years before the first symptoms appear," Jucker said. "The time period when therapies targeting beta-amyloid plaques are most effective thus appears to be earlier than what has been targeted in clinical trials to date. Future Alzheimer's therapies targeting beta-amyloid plaques should therefore definitely start earlier."
Originalpublikation
Experimental evidence for temporal uncoupling of brain Aβ deposition and neurodegenerative sequelae.
Rother et al.
Nature Communications, 13, 7333 (2022).
DOI: 10.1038/s41467-022-34538-5
