Ulm/Halle, April 13, 2023 – Two characteristic pathologies of Alzheimer's disease are related: Deposits of amyloid beta peptide in the brain and high levels of the synapse marker beta-synuclein in the blood appear together in Alzheimer's patients. This was discovered by an international research team, in which experts from the Ulm site of the German Center for Neurodegenerative Diseases (DZNE) and the Department of Neurology at the University Medicine Halle played a leading role. The scientists have now published their results in the renowned journal “Alzheimer's & Dementia: The Journal of the Alzheimer’s Association”.
The research team from Ulm and Halle had already shown a year ago in a highly regarded study that the beta-synuclein level in the blood is increased very early in the course of Alzheimer's disease. This indicates that synapses in the brain are damaged - a process that leads to cognitive impairment in patients. The current results are based on the first study: "We were able to show that the beta-synuclein level in the blood correlates with the amount of amyloid deposits in a variety of regions of the cortex," says PD Dr. Patrick Öckl, first author of the publication and researcher at the DZNE in Ulm. Scientists from the University Medicine Halle and the Center for Alzheimer Research in Stockholm were also involved in the study.
For their studies, the researchers drew on data from a cohort in Sweden: 126 subjects were studied in it - those with mild cognitive impairment as well as those with advanced dementia. "They all had a similar amount of amyloid deposits. These form very early in the course of the disease, even long before the first symptoms appear," says Prof. Dr. Markus Otto, Director of the Department of Neurology at the University Medicine Halle. Even in subjects with previously only mild cognitive impairment, the beta-synuclein level in the blood was already elevated. As the study showed, this could predict a later positive testing for amyloid deposits. The difference, however, lies in the complexity of the testing procedures: While blood tests - once developed - are easier to perform, detecting amyloid is incomparably more complex.
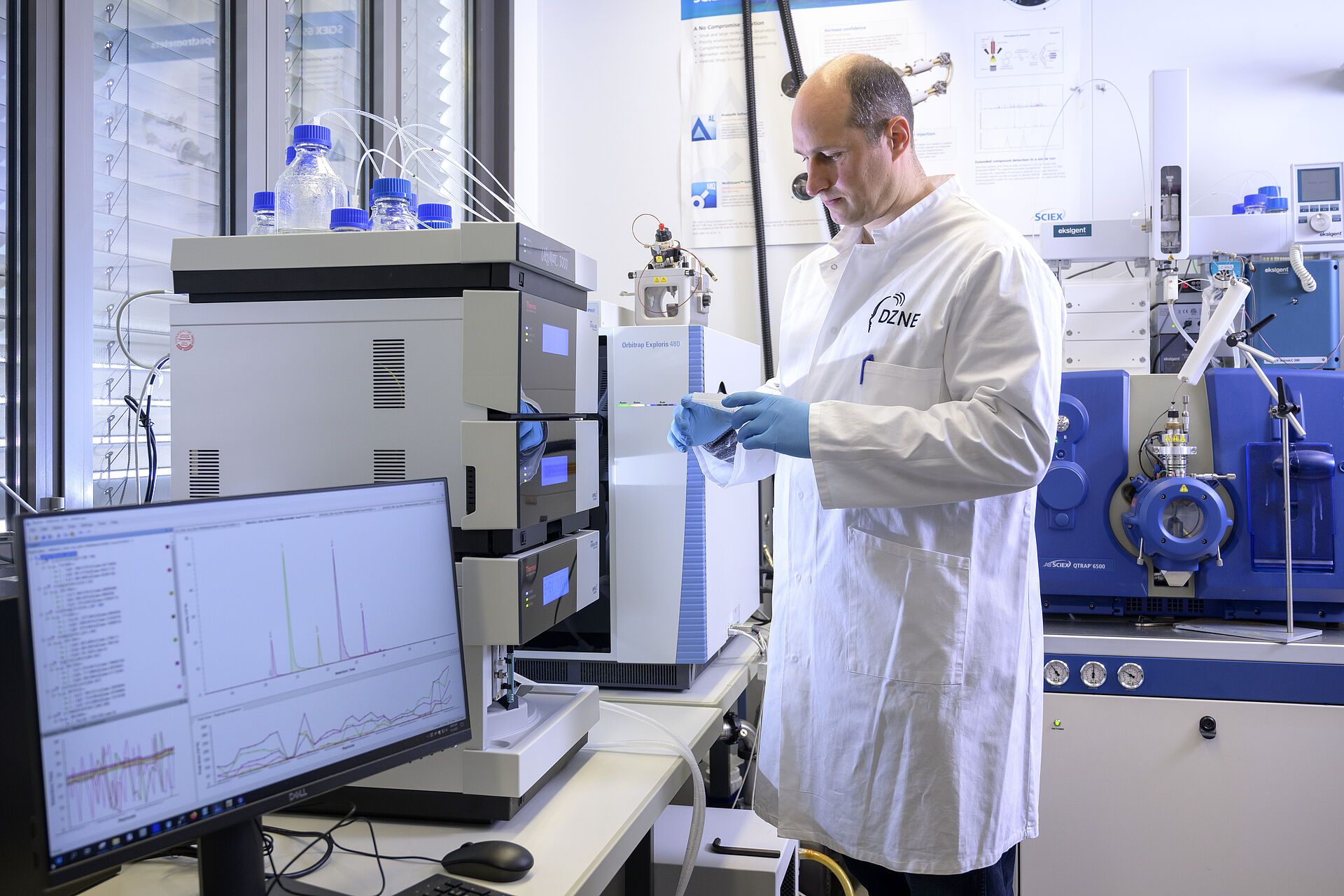
To determine how large the amyloid deposits are, the researchers used positron emission tomography. This high-tech examination allows the greatest possible precision. To measure the beta-synuclein level in the blood, they used mass spectrometry. Until now, beta-synuclein levels and other synapse markers could only be measured in cerebrospinal fluid. Taking these samples required a time-consuming and, for patients, often distressing CSF puncture. The fact that a blood test is now sufficient represents a considerable simplification of the examination.
The results of the Ulm and Halle researchers may help improve diagnostics. "Amyloid deposits form long before the onset of the first Alzheimer's symptoms. However, the presence of amyloid does not automatically mean that a patient also has Alzheimer's disease," says Patrick Öckl. So the question is when is the right time to start treatment. "Here, the beta-synuclein level could provide a clue: When synapse degeneration starts and thus the level rises, that could be a good moment."
The findings may also help studies assess how effective Alzheimer's therapies are. "Until now, cognitive impairment in Alzheimer's patients has been the yardstick for this," Öckl explains. If the deterioration of memory is halted or slows down, that was considered a success of a treatment. An indicator in the blood is a valuable addition. Öckl gives the Alzheimer's drug lecanemab, which made headlines last year, as an example: Clinical tests showed that patients had a sharp drop in the concentration of synaptic markers, similar to beta-synuclein, in their cerebrospinal fluid. If these results can be read in the blood instead of the cerebrospinal fluid, that is a significant advantage.
Original publication
Blood β-Synuclein is related to amyloid PET positivity in memory clinic patients, Patrick Oeckl et al., Alzheimer's & Dementia: The Journal of the Alzheimer's Association (2023)
DOI: 10.1002/alz.13046
April 2023